Me, to the doc who just saw my 45 year old patient presenting for two days of constipation: "Hey man, you want me to go ahead and call the fire department, or would you like to?"
Doc: "Uh, why exactly would we call for the FD?"
Me: Oh, well, you ordered an enema. I figured his butthole must be on fire, and I wanted to make sure that was taken care of by the appropriate people.
Doc: "Not funny."
Me: "Incorrect. That is hilarious. But the sentiment stands; I'm not doing a soap suds enema on this patient. You can change it to literally anything else, but unless I see flames I'm not going anywhere near him with that SSE."
***
I told the doc later that while I was in fact trying to be funny, I didn't want them to think I was blatantly ignoring their orders for the sake of being rude. I did, however, want them to recognize that ordering an enema as a first line constipation treatment on a completely healthy patient was ridiculous.
Seriously though, dude hadn't even taken a colace before coming in. He sure did get discharged with a bottle of mag citrate though, and NO ENEMA.
Tuesday, June 20, 2017
Monday, June 19, 2017
Gravity always wins
My feeling when, two minutes before my orientee and I get to clock out, our fall risk score of zero patient decides to faceplant off the end of the bed and I realize we now have another full hour of care/documentation to do:
 |
| Credit |
*for the record, he was totally fine
Thursday, June 15, 2017
Mistakes
It's easy to write about the times I felt good as a nurse, or did things easily, or was smart and caught some little detail that helped me better care for a patient. It's much more difficult to write about my failures.
This wasn't even a big mistake, just an offhanded comment that I've been ruminating over for weeks now.
Recently I had a kiddo with appendicitis who was being transferred to the pediatric hospital down the road. It was a ridiculously straightforward case: kid with zero medical history had no appetite for a day and then started with nausea and classic RLQ pain, parents brought him in for a workup, CT showed an appy and we started antibiotics and the transfer process. He was a typical young kid - old enough to know what was happening, but young enough to be terrified by it. About twenty minutes before transfer, he started to cry a bit.
What I should have done was sat down next to the kid and told him it was okay to be scared, that it was okay to cry. I should have validated his feelings and told him that yes, surgery is scary and doctors in masks can be scary and that this whole thing is scary - even me, trying to be comforting, can be scary.
I didn't.
Instead, I told him that it's okay, he doesn't need to be scared, that we're going to take great care of him and everything would be fine.
I can't make that promise - what if everything is not fine? I'll take care of him to the best of my ability, but he might still hurt. I'm not scared by hospitals, but he damn sure was. I told him the classic caregiver lie - with the best intentions and hopefully true, but not at all what a nine year old needs to hear.
I messed up.
This wasn't even a big mistake, just an offhanded comment that I've been ruminating over for weeks now.
Recently I had a kiddo with appendicitis who was being transferred to the pediatric hospital down the road. It was a ridiculously straightforward case: kid with zero medical history had no appetite for a day and then started with nausea and classic RLQ pain, parents brought him in for a workup, CT showed an appy and we started antibiotics and the transfer process. He was a typical young kid - old enough to know what was happening, but young enough to be terrified by it. About twenty minutes before transfer, he started to cry a bit.
What I should have done was sat down next to the kid and told him it was okay to be scared, that it was okay to cry. I should have validated his feelings and told him that yes, surgery is scary and doctors in masks can be scary and that this whole thing is scary - even me, trying to be comforting, can be scary.
I didn't.
Instead, I told him that it's okay, he doesn't need to be scared, that we're going to take great care of him and everything would be fine.
I can't make that promise - what if everything is not fine? I'll take care of him to the best of my ability, but he might still hurt. I'm not scared by hospitals, but he damn sure was. I told him the classic caregiver lie - with the best intentions and hopefully true, but not at all what a nine year old needs to hear.
I messed up.
Monday, June 12, 2017
Vitals
I went in to discharge a patient last night, and since she had been there a little over two hours I needed to check a set of discharge vitals. I opened a new cuff and p-ox and let them run while I was going over the paperwork, then wrote down the vitals and waved her off to the exit. Back at my computer to chart all the discharge paperwork, I noticed that the blood pressure and heart rate I had just taken were the exact same as the triage set. Does anyone else ever get that weird feeling when this happens that if your chart gets audited, whoever is reading over it will scoff and be like "chyeah, obviously they didn't check discharge vitals! No one has a repeat BP of 143/68 and HR of 71! I'm definitely going to call them in for a meeting."
I then had a moment of questioning if I should change it by just a single number, to 142/68 or something, just enough to make it different and clearly a new set of vitals. Or even to chart the correct identical BP/HR, but free text a note that yes, they are in fact a new set. Which then led to me feeling horribly guilty for even thinking about falsifying data, but also wondering if I'm just a crazy person simply for having this series of thoughts.
Paranoia over chart auditing is such a weird thing.
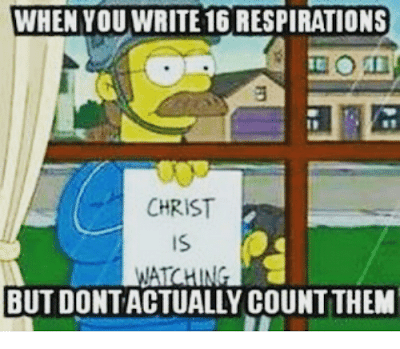
And then I remembered that everyone, everywhere, always charts 16 as the RR (edit: in the stable, non-respiratory or neuro patients. I'm not that shitty of a nurse; geeze, guys!) and then I felt better about myself.
I then had a moment of questioning if I should change it by just a single number, to 142/68 or something, just enough to make it different and clearly a new set of vitals. Or even to chart the correct identical BP/HR, but free text a note that yes, they are in fact a new set. Which then led to me feeling horribly guilty for even thinking about falsifying data, but also wondering if I'm just a crazy person simply for having this series of thoughts.
Paranoia over chart auditing is such a weird thing.
And then I remembered that everyone, everywhere, always charts 16 as the RR (edit: in the stable, non-respiratory or neuro patients. I'm not that shitty of a nurse; geeze, guys!) and then I felt better about myself.
 |
| photo credit |
Wednesday, June 7, 2017
Personal Best
So guys I hit my personal all time-best record of AMA discharges yesterday. I had, count em', one two three FOUR against medical advice discharges! Four! And two of those came literally at the same time, with adjacent rooms both signing out (no, they weren't there together). I did my part in legitimately trying to get the one guy who needed to stay refrain from signing out, but no dice. The other three I practically tripped over myself to get the paperwork ready so I could hold the door open for them.
I very nearly had a fifth AMA, but the admit doctor swooped in at the last second and convinced her to stay. Le sigh. Coulda had the championship thumb ring, but at least tonight is another chance!
I very nearly had a fifth AMA, but the admit doctor swooped in at the last second and convinced her to stay. Le sigh. Coulda had the championship thumb ring, but at least tonight is another chance!
Subscribe to:
Posts (Atom)